Introduction
Vitamin D plays an important role in bone homeostasis. It enhances the absorption of the minerals calcium and phosphate (which are the main building blocks of bone) and magnesium. Additionally, vitamin D deficiency has been associated with countless autoimmune diseases, cancers and cardiovascular disease [1]. Severe vitamin D deficiency can also drastically impact muscle strength and health [2]. Notably, some evidence indicates that vitamin D levels above what is considered sufficient might increase sports performance, muscle strength and muscle hypertrophy [3, 4].
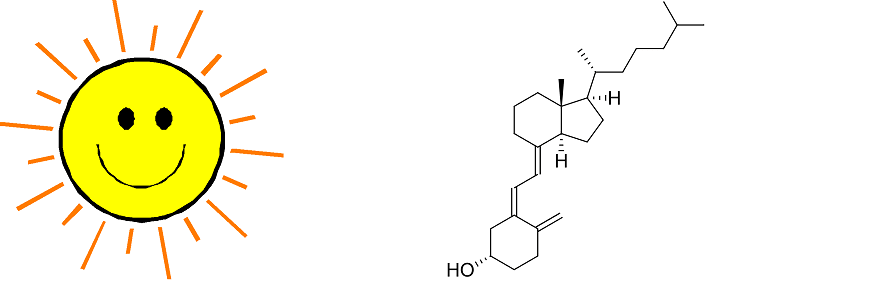
Vitamin D can be synthesized by the human body when exposed to sunlight. More specifically, ultraviolet B (UVB) rays. It can also be found in the diet. Although the quantities in food are usually (very) small. Some exceptions to this are fatty fish, such as salmon, mackerel and herring [5]. Very small amounts can also be found in meat. An overview of the vitamin D contents of some foodstuffs are given in the table below.
| Foodstuff | Vitamin D (IU/100 g) |
|---|---|
| Wild salmon | 996 |
| Farmed salmon | 242 |
| Mackerel | 24 - 440 |
| Herring | 1.100 |
| Eel | 560 - 1.072 |
| Chicken | ~10 |
| Pork | ~10 |
| Beef | ~10 |
Because it isn’t common in food, some dietary products are fortified with vitamin D. This is most commonly done with milk and baking and frying products. In my country (the Netherlands) for example, some baking and frying products are fortified with vitamin D up to 300 IU/100 g. (Which of course still is quite low.)
Vitamin D is usually well absorbed from the diet
Two forms of vitamin D can be found in the diet: vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol). Vitamin D2 hardly occurs in the diet, with the exception of some mushroom species, supplements and fortified foods. Vitamin D3 however is the form you’ll find in all animal sources of vitamin D. A lot of dietary supplements also contain vitamin D3.
Vitamin D is primarily absorbed in the small intestine, specifically the ileum and jejunum [7]. The amount absorbed ranges from 55 to 99%, with an average of 78% [7]. Absorption occurs both passively by diffusion, as well as by transporters [8]. Cholesterol transporters in particular seem to be involved with this.
Vitamin D might be better absorbed when taken together with a fatty meal
A study suggests that vitamin D is better absorbed when taken together with a fatty meal compared to a fat-free meal [9]. The absorption does not seem to be affected by the concentration of monounsaturated versus polyunsaturated fatty acids in it. It’s uncertain what the minimum amount of fat would be for optimal absorption. I suppose a few grams would be enough. (The trial compared a meal containing 30 g fat to a meal containing 0 g fat.)
Given that it’s quite well absorbed even with a no-fat meal, it’s more of a gimmick to take your vitamin D with a fatty meal.
Many people are vitamin D-deficient
Vitamin D deficiency is very prevalent around the globe. As the renowned vitamin D researcher Michael Holick wrote:
“Vitamin D deficiency and insufficiency is a global health issue that afflicts more than one billion children and adults worldwide." [10]
Indeed, this is also the case for my country. For example, a study found that the majority (50-80%) of the Dutch elderly population is vitamin D deficient [11]. Similar numbers are found among Dutch athletes. A study with Dutch athletes found 34% to be vitamin D deficient and 36% to be vitamin D insufficient [12].
Reference ranges for a deficient, insufficient and adequate vitamin D status by the Endocrine Society are provided in the table below [13]. (Note that vitamin D is measured in the blood as its metabolite 25(OH)D.)
| Vitamin D status | Serum 25(OH)D concentration |
|---|---|
| Deficient | <50 nmol/L |
| Insufficient | 52.5 - 72.5 nmol/L |
| Adequate | >75 nmol/L |
It should not come as a surprise that it’s so prevalent. Most people would need to rely on sun exposure for sufficient vitamin D if they aren’t supplementing it. This is exceedingly problematic in countries with little sunlight hours and those at high latitude. For example, in Boston (42.2 degrees N), you won’t produce vitamin D from November through February [14]. The UV radiation would be too weak. Further north, in Edmonton (but also the Netherlands for example, 52 degrees N), this period extends from October through March. This is also named ‘vitamin D winter’.
Additionally, older age, a darker skin pigment and sunscreen use can lower the amount of vitamin D produced by sunlight.
How much vitamin D should you supplement?
This will largely depend on your initial vitamin D levels. A study in young and elderly men showed an increase from 41.3 to 74.1 and 70.7 to 111.2 nmol/L, respectively, after 16 weeks supplementation with 1.920 IU vitamin D3 daily [15]. So expect an increase of roughly 35 nmol/L when supplementing about 2.000 IU daily. This is also in accordance with other literature I’ve read. This is likely enough for quite some, but not all, people to get in the adequate range.
Given that a risk analysis by Hathcock et al. puts the highest dosage at which no adverse effects occur at 10.000 IU vitamin D3 daily [15], and the - conservative - European Food and Safety Authority (EFSA) has put the tolerable upper limit of intake at 4.000 IU daily [16], you can safely assume that you can take 4.000 IU daily without worries of any toxicity at all.
So it basically boils down to supplementing 2.000 to 4.000 IU vitamin D daily, and you’re fine. Sit at the higher end if you come outside rarely, sit at the lower end if you do catch some frequent sunrays. (Forget supplementing if you get a lot of sunlight.)
As a final note, it doesn’t matter that much whether you supplement with vitamin D3 or vitamin D2, but D3 has shown to be the most effective of the two in raising serum 25(OH)D concentration [17].
References
- Holick, Michael F. "Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease." The American journal of clinical nutrition 80.6 (2004): 1678S-1688S.
- Dawson-Hughes, Bess. "Vitamin D and muscle function." The Journal of steroid biochemistry and molecular biology 173 (2017): 313-316.
- Abrams, Geoffrey D., David Feldman, and Marc R. Safran. "Effects of vitamin D on skeletal muscle and athletic performance." JAAOS-Journal of the American Academy of Orthopaedic Surgeons 26.8 (2018): 278-285.
- Książek, Anna, Aleksandra Zagrodna, and Małgorzata Słowińska-Lisowska. "Vitamin D, skeletal muscle function and athletic performance in athletes—A narrative review." Nutrients 11.8 (2019): 1800.
- Holick, Michael F. "Vitamin D in health and disease: Vitamin D for health and in chronic kidney disease." Seminars in dialysis. Vol. 18. No. 4. Oxford, UK: Blackwell Science Inc, 2005.
- Schmid, Alexandra, and Barbara Walther. "Natural vitamin D content in animal products." Advances in nutrition 4.4 (2013): 453-462.
- Reboul, Emmanuelle. "Intestinal absorption of vitamin D: from the meal to the enterocyte." Food & function 6.2 (2015): 356-362.
- Reboul, Emmanuelle, et al. "Vitamin D intestinal absorption is not a simple passive diffusion: evidences for involvement of cholesterol transporters." Molecular nutrition & food research 55.5 (2011): 691-702.
- Dawson-Hughes, Bess, et al. "Dietary fat increases vitamin D-3 absorption." Journal of the Academy of Nutrition and Dietetics 115.2 (2015): 225-230.
- Holick, Michael F. "The vitamin D deficiency pandemic: approaches for diagnosis, treatment and prevention." Reviews in Endocrine and Metabolic Disorders 18.2 (2017): 153-165.
- Wielders, Jos PM, Frits AJ Muskiet, and Albert van de Wiel. "Nieuw licht op vitamine D: herwaardering van een essentieel prohormoon." Nederlands tijdschrift voor geneeskunde 154.49 (2010): 2271-2276.
- Backx, E. M. P., et al. "The impact of 1-year vitamin D supplementation on vitamin D status in athletes: a dose–response study." European journal of clinical nutrition 70.9 (2016): 1009-1014.
- Holick, Michael F., et al. "Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline." The Journal of Clinical Endocrinology & Metabolism 96.7 (2011): 1911-1930.
- Webb, Ann R., L. Kline, and Michael F. Holick. "Influence of season and latitude on the cutaneous synthesis of vitamin D3: exposure to winter sunlight in Boston and Edmonton will not promote vitamin D3 synthesis in human skin." The journal of clinical endocrinology & metabolism 67.2 (1988): 373-378.
- Hathcock, John N., et al. "Risk assessment for vitamin D." The American journal of clinical nutrition 85.1 (2007): 6-18.
- EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA). "Scientific opinion on the tolerable upper intake level of vitamin D." EFSA Journal 10.7 (2012): 2813.
- Tripkovic, Laura, et al. "Comparison of vitamin D2 and vitamin D3 supplementation in raising serum 25-hydroxyvitamin D status: a systematic review and meta-analysis." The American journal of clinical nutrition 95.6 (2012): 1357-1364.